The human body’s substantial spine framework is made of plate of cells along the back of a nascent life form (called the neural plate). Right on time being created, the edges of this plate begin to contort up toward each other, making the neural tube—a limited sheath that closes to shape the psyche and spinal line of the hatchling. As change advances, the most elevated purpose of the tube transforms into the brain and whatever remains of the spinal rope. This methodology is by and large wrapped up by the 28th day of pregnancy. Nevertheless, if issues happen in the middle of this method, the result can be cerebrum issue called neural tube flaws, including spina bifida.
Spina bifida, which really means "split spine," is portrayed by the insufficient headway of the brain, spinal rope, and/or meninges (the cautious covering around the cerebrum and spinal string.
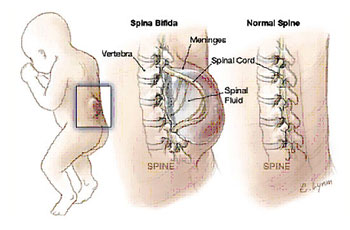
There are four sorts of spina bifida: occulta, shut neural tube imperfections, meningocele, and myelomeningocele. Occulta is the mildest and most normal frame in which one or more vertebrae are distorted. The name "occulta," which signifies "concealed," demonstrates that a layer of skin covers the abnormality, or opening in the vertebrae. This type of spina bifida, display in 10-20 percent of the overall public, seldom causes inability or indications.
Shut neural tube deformities make up the second kind of spina bifida. This structure comprises of a differing gathering of imperfections in which the spinal line is stamped by contortions of fat, bone, or meninges. In many occasions there are few or no side effects; in others the deformity causes fragmented loss of motion with urinary and gut brokenness.
In the third sort, meningocele, spinal liquid and meninges project through an anomalous vertebral opening; the abnormality contains no neural components and could possibly be secured by a layer of skin. A few people with meningocele may have few or no manifestations while others may experience such side effects as complete loss of motion with bladder and inside brokenness.
Myelomeningocele, the fourth frame, is the most serious and happens when the spinal rope/neural components are uncovered through the opening in the spine, bringing about incomplete or complete loss of motion of the parts of the body beneath the spinal opening. The impedance may be severe to the point that the influenced individual is not able to walk and may have bladder and gut brokenness.
The indications of spina bifida fluctuate from individual to individual, contingent upon the sort and level of association. Shut neural tube deformities are regularly perceived right on time in life because of an unusual tuft or cluster of hair or a little dimple or pigmentation on the skin at the site of the spinal contortion.
Meningocele and myelomeningocele for the most part include a liquid filled sac—unmistakable on the back—jutting from the spinal waterway. In meningocele, the sac may be secured by a meager layer of skin. Much of the time of myelomeningocele, there is no layer of skin covering the sac and a territory of anomalous created spinal line tissue is typically uncovered
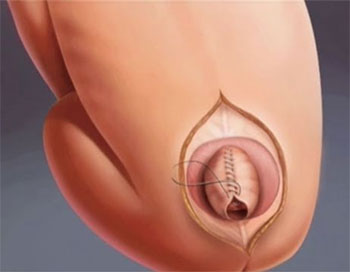
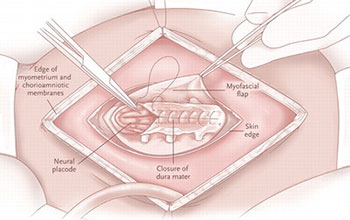
Surgery for spina bifida includes a mixed bag of neurosurgical, orthopedic, and urologic strategies. Surgical methodology incorporates the accompanying:
Without conclusion of the imperfection, survival is endangered. Conclusion may turn out to be all the more much of the time a pre-birth strategy.
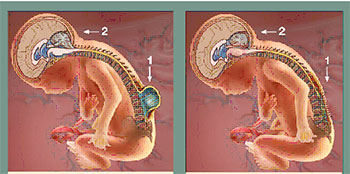
Some have seen the association between spina bifida and hydrocephalus in a brought together sense, such that spina bifida is an outcome of fetal hydrocephalus.
Past conclusion, other required neurosurgical strategies may incorporate shunting for hydrocephalus, including ordinary weight hydrocephalus. Numerous urologic strategies may be needed for the neurogenic bladder.
Spinal distortion is regular in patients with spina bifida and is extremely hard to treat. On the other hand, amendment and combination are important to capture movement and entanglements and are requirements for fruitful treatment of lower-furthest point distortions and for lessening of impedances to strolling and sitting. The writing has neglected to report a critical personal satisfaction change with combination.
Disease is regular, especially in spina bifida patients with a neurogenic bladder. An expanded danger exists with any agent system. Retethering of the spinal string every now and again happens and may show urologically and orthopedically. Any suspected change in muscle status, which must be observed serially, or urologic status may be an indication of retethering.
Spinal deformation recreation may be especially difficult due to back component insufficiencies. These can prompt instrumentation and combination disappointments, disease from the neurogenic bladder, and distal ulcers from insensate skin. Front techniques are being joined all the more every now and again with the back way to deal with produce a palatable combination.
Lower-limit systems are required by muscle unevenness powers. Sentiments vary in the matter of whether they help in seating and ambulation. Walk examination has been utilized to break down particular applicants who have engine quality in the quadriceps in the scope of "good in addition to" and who likewise have hip dysplasia or separation.
Techniques distal to the hip frequently are like those for polio yet for the most part are gone for keeping up the capacity to support the appendage to augment openness and autonomy. These techniques are coordinated toward lessening deformation, discharging contractures, and adjusting muscle powers from the variable neurologic sores.